Low Sperm / Abnormal Sperm
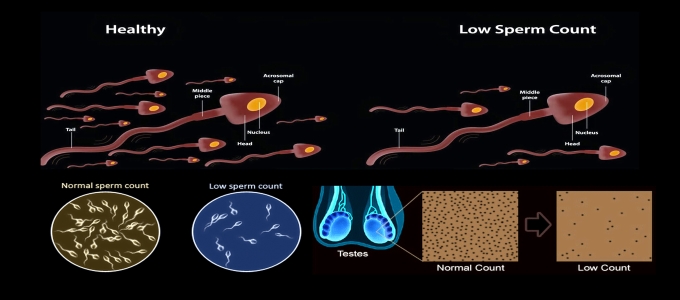
Low sperm count means that the fluid (semen) you ejaculate during an orgasm contains fewer sperm than normal. A low sperm count is also called oligospermia. A complete absence of sperm is called azoospermia. Your sperm count is considered lower than normal if you have fewer than 15 million sperm per milliliter of semen.
Having a low sperm count decreases the odds that one of your sperm will fertilize your partners egg, resulting in pregnancy. Nonetheless, many men who have a low sperm count are still able to father a child.
The main sign of low sperm count is the inability to conceive a child. There might be no other obvious signs or symptoms. In some cases, an underlying problem such as an inherited chromosomal abnormality, a hormonal imbalance, dilated testicular veins or a condition that blocks the passage of sperm may cause signs and symptoms.
Pretesticular azoospermia
- Problems with sexual function — for example, low sex drive or difficulty maintaining an erection (erectile dysfunction)
- Pain, swelling or a lump in the testicular area
- Decreased facial or body hair or other signs of a chromosome or hormone abnormality.
Semen
Male Factor :
Semen– Human semen is 3-5 ml white liquid containg 40-100 million sperms. When sperms count is good the semen has a good viscocity. If there no sperms the semen is thin and watery. Soon after ejaculation the semen is viscous and in 5-10 mins it liquifes. When there is infection it is yellow in colour. Some men have ejaculatory dysfunction where the help of a sexual medicine doctor is taken. Common problem in semen are
- low count – Oligospermia
- Pus cells – Pyospermia
- Low motility – Astheno Spermia
- Dead sperms – Necro spermia
- No sperms – Azoo spermia
Normal sperm has > 40 million count , > 50% motile , ( grade 4 ) no pus cells , no becteria
Sperms are produced in testis in highly colied tubes called Seminiferous Tubules. If we take a cut section of the seminiferous tubules we will find a layer of cells ( maturing spermatozoa ) in the cavity are seen sperms a sperm has head , neck , middle piece , tail.
All seminiferous tubules open in a singal duct called Epididymus and sperms are carried through this tube in to another tube calle VAS DEFERENS to the male urethra. If there is a block any where in this route ( Epididymus to Vas Deferens ) even though the testis are producing sperms no sperms will be seen in the semen this is called OBSTRUCTIVE AZOOSPERMIA. In such men testicular size and consistency is normal but no sperm seen in semen. If we check the hormones : FSH + LH there serum levels are normal. These men can have baby with there sperms by using ICSI technique. Sperm are aspirated from the testis using a fine needle and used in ICSI technique.
In some Azoospermic men testis are small and hard in consistency serum FSH is high and the testis have no seminiferous tubules or cells in the tubules ( non obstructive azoospermia ) occasionally an open biopsy a few sperms may be found in some tubules which can be use for ICSI technique.
When sperm count is < 5 million the cause may be a problem in the males chromosomes or genes or it could be due to some testicular infection in the past ( Mumps )
For a very low count a man must get his Karyotype ( Study of Chromosomes ) done.
If semen has many pus cells then culture and sensitivity should be done and a rigorous treatment with Antibiotics should be done. ICSI is the best treatment for these patients than IVF. As there is a risk of bacterial growth in the cuture media.
Astheno Spermia : Normally sperms are highly motile cells the move so rapidly that there tail cannot be visualised. Sometimes due to heat , toxins , genetic problems sperm motility is decreased. Such sperms cannot naturally fertilise an egg. ICSI is the treatement of choice.
Terato spermia : Sometimes sperms may have abnormal morphology like
- tail defect.
- middle piece defect.
- neck defect.
- head & achrosomic cap defect.
Many of these defects have minor significance and hence these sperms can be used for ICSI. Only when NECK DEFECT are seen donor sperms are advisable as the NECK has centrosomes which are required for cell division after fertilization.
How Can You Remove Sperms Form Testis In Obstructive Azoo Spermia ?
- Mesa : Meso Epididymal Sperm Aspiration.
- TESA : when tha sperm are aspirated from the testis with a needle it is called TESTICULAR SPERM ASPIRATION ( TESA ).
- PESA : when the sperm are removed from Epididymis it called PER CUTANEOUS EPIDIDYMAL SPERM ASPIRATION ( PESA ).
- MICRO TESE : when testis are cut and seminiferous tubules are pulled out and cannulaed to aspirate the sperm with the help of operating microscope it is call MICRO TESE. ICSI has revolutionized the treatement of male infertility even a few sperms are enough to produce embryos.
Common Test Done In An Infertile Couple :
1) semen analysis – Husbund gives his semen after 2 days of abstinence by masturbation. If the semen sample is brought frmon home it should reach the lab within 1 hour. If sample collection is difficult by masturbation than semen sample can be collected by special condoms and natural intercourse.
2) Trans vaginal ultrasound. ( TVS ) – Ultrasound is a techonology by which sound waves by high frequency > 2megha hertz pass through the soft tissues and according to there consistencies sound wave are echoed back to the transducer and images are displed on the monitor. TVS probes are of 5-7.5-10 MHz and we can see uterus , endometrium ovaries , fluid filled cysts. This is the best non invasive investigation giving maximum information about the pelvis. It is very useful in IVF for follicular study and oocyte aspiration.
Follicular study : It is the study of monitoring ovarin follicles and the day of ovulation with the help TVS probe for planned intercourse and IUI. It is done when tablets and injection of FSH / HMG are used for ovulation induction.
Ovum pickup : with the help of TVS probe follicles can be aspirated under anesthesia with the help of a needle. This is called Ovun Pickup.
HSG ( HYSTERO SALPINGO GRAPHY ) : Is a test done to check the patency of fallopian tubes , shape of the uterine cavity with the help of the Radio Opaque dye pushed in the uterine cavity and x-ray film’s are taken. They show the inner lining of uterus, tube and spillage of the dye in the peritoneal cavity it is done without done anestheisa.
LAPROSCOPY : Always done under anesthesia is an Invasive procedure where a key hole is made at the umbilicus and a scope is passed to visualise the uters tubes ovaries. It can be extended to do any corrective surgery like removal of adhesions or ovarian cysts.
HYSTERO SCOPY : Here we visualise the uterine cavity the Ostia by passing a scope through the cervix.
Azoospermia

Azoospermia may occur because of reproductive tract obstruction (obstructive azoospermia) or inadequate production of spermatozoa, such that spermatozoa do not appear in the ejaculate (non-obstructive azoospermia). Azoospermia is diagnosed based on the absence of spermatozoa after centrifugation of complete semen specimens using microscopic analysis.
Azoospermia can be classified into three major types as listed. Many conditions listed may also cause various degrees of oligospermia rather than azoospermia.
Pretesticular azoospermia
Pretesticular azoospermia is characterized by inadequate stimulation of otherwise normal testicles and genital tract. Typically, follicle-stimulating hormone (FSH) levels are low (Hypogonadotrophic) commensurate with inadequate stimulation of the testes to produce sperm. Examples include hypopituitarism (for various causes), hyperprolactinemia, and exogenous FSH suppression by testosterone. Chemotherapy may suppress spermatogenesis. Pretesticular azoospermia is seen in about 2% of azoospermia
Testicular azoospermia
In this situation the testes are abnormal, atrophic, or absent, and sperm production severely disturbed to absent. FSH levels tend to be elevated (hypergonadotropic) as the feedback loop is interrupted (lack of feedback inhibition on FSH). The condition is seen in 49-93% of men with azoospermia. Testicular failure includes absence of failure production as well as low production and maturation arrest during the process of spermatogenesis.
Causes for testicular failure include congenital issues such as in certain genetic conditions (e.g. Klinefelter syndrome), some cases of cryptorchidism or Sertoli cell-only syndrome as well as acquired conditions by infection (orchitis), surgery (trauma, cancer), radiation,[3] or other causes. Mast cells releasing inflammatory mediators appear to directly suppress sperm motility in a potentially reversible manner, and may be a common path physiological mechanism for many causes leading to inflammation. Generally, men with unexplained hypergonadotropic azoospermia need to undergo a chromosomal evaluation.
Post testicular azoospermia post testicular azoospermia sperm are produced but not ejaculated, a condition that affects 7-51% of azoospermic men. The main cause is a physical obstruction (obstructive azoospermia) of the post testicular genital tracts. The most common reason is a vasectomy done to induce contraceptive sterility. Other obstructions can be congenital (example agenesis of the vas deferens as seen in certain cases of cystic fibrosis) or acquired, such as ejaculatory duct obstruction for instance by infection.
Ejaculatory disorders include retrograde ejaculation and an ejaculation; in these conditions sperm are produced but not expelled.
Idiopathic azoospermia
Idiopathic azoospermia is where there is no known cause of the condition. It may be a result of multiple risk factors, such as age and weight. For example, a review in 2013 came to the result that oligospermia and azoospermia are significantly associated with being overweight (odds ratio 1.1), obese (odds ratio 1.3) and morbidly obese (odds ratio 2.0), but the cause of this is unknown. The review found no significant relation between oligospermia and being underweight.
DNA Fragmentation Index

Sperm DNA fragmentation
The genetic integrity of the spermatozoan is essential for normal embryo development. A high level of DNA fragmentation in sperm cells may represent a cause of male infertility that conventional examinations – sperm concentration, motility analysis, morphology assessment – cannot detect. Results reported in the scientific literature show regardless of the assisted reproductive technology used, elevated levels of DNA fragmentation above the critical threshold will significantly compromise the possibility of a successful pregnancy.
High sperm DNA fragmentation does not appear to affect fertilisation or the first or second embryo cleavage stages
High sperm DNA fragmentation can affect embryo cleavage once the paternal genome is switched on, and subsequent blastocyst development
DNA fragmentation levels are closely correlated with IUI, IVF and ICSI miscarriage and pregnancy rates
DNA fragmentation is significantly higher in sub fertile men.
Men with poor semen parameters are more likely to have high DNA fragmentation
High sperm DNA fragmentation is also found in men with normal semen parameter
Teratospermia
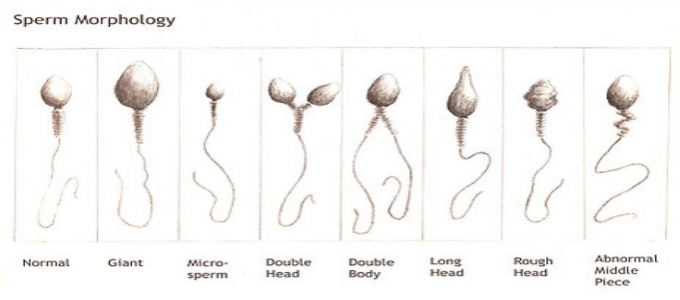
Teratozoospermia, also known as teratospermia, is a semen alteration in which there is a large number of spermatozoa with abnormal morphology.It is a sperm condition that may lead to serious consequences, such as male infertility. The sperm parameter that is compromised is sperm morphology. The World Health Organisation (WHO) offers guidelines to evaluate semen parameters (some examples of these parameters are concentration, motility, or morphology). The values set by WHO can be used to determine normality, so if the value of a given semen parameter is below the reference, it may suggest a sperm pathology. With regard to teratozoospermia, the shape of the spermatozoon is assessed. Formerly, teratozoospermia was diagnosed if 14% of the sperm had a normal shape. In 2010, WHO updated its reference values, and now a man only has to meet a 5% rate of properly shaped spermatozoa to be within normality. Therefore, in order to diagnose teratozoospermia by the current standards, a man has to show a high rate of dysfunctional spermatozoa; more than 96% of his spermatozoa have to be morphologically abnormal.
Y-Microdeletion
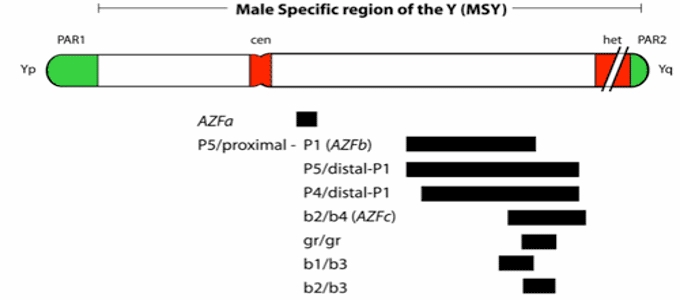
Y chromosome microdeletion (YCM) is a family of genetic disorders caused by missing gene(s) in the Y chromosome. Many men with YCM exhibit no symptoms and lead normal lives. However, YCM is also known to be present in a significant number of men with reducedfertility. Men with reduced sperm production (in up to 20% of men with reduced sperm count, some form of YCM has been detected) varies from oligozoospermia, significant lack of sperm, or azoospermia, complete lack of sperm.
Klinefelters System

Klinefelter syndrome is a chromosomal condition that affects male physical and cognitive development. Its signs and symptoms vary among affected individuals.
Affected individuals typically have small testes that do not produce as much testosterone as usual. Testosterone is the hormone that directs male sexual development before birth and during puberty. A shortage of testosterone can lead to delayed or incomplete puberty, breast enlargement (gynecomastia), reduced facial and body hair, and an inability to have biological children (infertility). Some affected individuals also have genital differences including undescended testes (cryptorchidism), the opening of the urethra on the underside of the penis (hypospadias), or an unusually small penis (micropenis).


